In August, (one month ago today)I had an appendectomy. There was very little drama involved, the doctors office visit led straight to a same day CT scan and an emergency review with the radiologist who informed me the appendix couldn't be seen but the colon was most definitely inflamed and I should go to the ER if it got worse. To the ER I went that night, to a hospital where the D Care is very good (had that going for it). They admitted me under observation, coursing enough pain medications through me to make me sick for the next 14 hours. The plan was to do another CT the next day. In observation, as I was trying not to move or vomit the admitting nurse asked a zillion questions and many of them were about the pump and the hospital "contract"
to continue my pump, but use their insulin/check with their meter,tell them all boluses/set changes, etc. It wasn't a big deal to me(indeed, I'd much prefer my pump then going off on something else) so I agreed. When morning came, they sent me off for another CT & the movement from that even in the bed made me sick again. Surgeons and the PA came in again, they still couldn't see my appendix & recommended removal.(well,surgery did. I cried and told them I didn't know so they said they'd come back.) The PA came in and told me not to let surgery talk me into something I didn't want & if I got it, I should know why I was getting it and they were going to try to work on the pain and nausea regardless so protonix and Zofran and Reglan were administered and that made me conk out for over an hour and when I woke up, the nausea was much better. Not so much the pain. I talked to the nurse and the PA again and decided I would go ahead with surgery, it could only help. Surgery came back at 8,& told me they'd do it at 11 the next morning, there were many emergent cases that evening. In the meantime, I could have clear fluids, so I had some watery broth and water. Morphine straight up made me sicker then a dog so I chose the other form of pain control. At 9 pm I had a low and had to have juice,at 12:30 I had another low. (12 was supposed to be NPO) At 8:30 am had another low and my nurse had to ask the doc what to do (ultimately pushing dextrose through my IV, which took me to 200 very fast) There was then another OR delay and I was told it would be 1 pm before it happened. And then I heard people talking to other people and "she's on a pump" being said and magically, it was back to 11 am.(yay for diabetes pushing me back up the list.) They took me to the OR then, and the OR nurse and anesthesiologist popped in to go over anything untoward and confirm pump/CGM placement. My bg was back down to 93 so the anesthesiologist told me to turn my pump off because he was worried about lows.(I didn’t. I put it at 0.0 for two hours, so I wouldn’t go into DKA) Some dextrose (D5) was still running through my IV. They pushed sedating meds through the IV and it’s weird the feeling you get when you’re going under, kind of ditzy and then you are out cold, dreaming weird stuff and just like that you’re awake again in the post-surgical unit, trying to figure out what happened & oh yeah, there are incisions in my abdomen and do I feel sick or in pain as you are coming out of the anesthesia haze. I didn’t. Just tired. The anesthesiologist did a good job of giving adequate amounts of nausea/pain meds, because nausea is a common thing with me after surgery.(I’d told him in advance this was a problem and he said he’d give me extra) Bg was 143 and steady.(kept Dex/PDM with me,sent everything else with security)I was expecting to be discharged after it wore off, instead they took me up to a surgical unit. So then I assumed I’d stay the night. There was a flurry of activity by the nurse and tech after I was wheeled up to the unit, nausea and more pain meds given, and the pillow became my best friend for splinting during coughing. By 8 pm another surgical resident came by and told me I could go home since it was uncomplicated. I told him there was no way I was going home that night, couldn’t eat anything (throw in diabetes and tanking electrolyte levels) & if he looked harder, he could find a reason to keep me admitted. He said he couldn’t force me to leave but the insurance co might not pay. I said I was going to take that chance. I then tried to eat a chicken salad sandwich (on his suggestion) and the pain of the three bites I could get down had me writhing for the next few hours. My throat was dry and my kidneys were on overdrive. Next morning, the PA said I could go home after getting IV magnesium and potassium(right on cue, those levels were dropping low as well). At 4 pm, she came in, asked how I was feeling (great!yay!) and then said I couldn’t go home because my creatinine had jumped 0.5 in a day and I was dehydrated from urinating so much. I had just thought it was par for the course from all those surgery drugs. Insurance company reason for admittance: solved. That required a bunch more IV fluids and drinking a bunch more overnight/morning.
Next day: all labs back to normal, discharged that evening.
I think that one of the strangest parts of that very strange experience was crossing the "doesn't need to be on blood thinners" to "prescribed blood thinning (heparin) injections" twice daily line..not even during pregnancy was I on blood thinners(granted, I was 30 then, not almost 36.) Nurse # 1 casually dropped that bombshell before surgery and I had to fully process that fact that I was now of the age where this could be a thing. I said no, but I wore the SCD's and TEDS and ambulated because blood clots still needed preventing. By the next day I was post surgery and admitted to the floor and a new nurse came to give me the shot and I agreed because she was just like "you need this" and I was also thinking she was probably right.I was nervous getting it but it did nothing unusual. This nurse also knew that I was a nurse (she must have read the chart,or it was mentioned during report or something) because none of the other floor nurses talked nurse stuff to me as she did. I didn't particularly feel like talking about my career(although the PA and NP kind of drug it out of me), when you don't feel well you just want to stay in bed and not talk. So, after that, I got the prescribed twice a day heparin injections until getting out of the hospital 2 days later. Thinner blood is much preferable to having a clot. Something else I've learned regarding being NPO and my labs, my magnesium will decrease at the rate of 0.1 per day with no oral magnesium intake-and the potassium will likewise be low. Before and after surgery I had to get potassium IV bags. More then anything else, this throws wrenches in the whole discharge thing they do not like when your potassium is going down. Magnesium and potassium going low easily are always going to be an issue for me,& moving forward I need to A.keep my supplements with me and B. take potassium occasionally,along with high potassium foods on a regular basis. Because of Mody magnesium is just as vital as insulin.
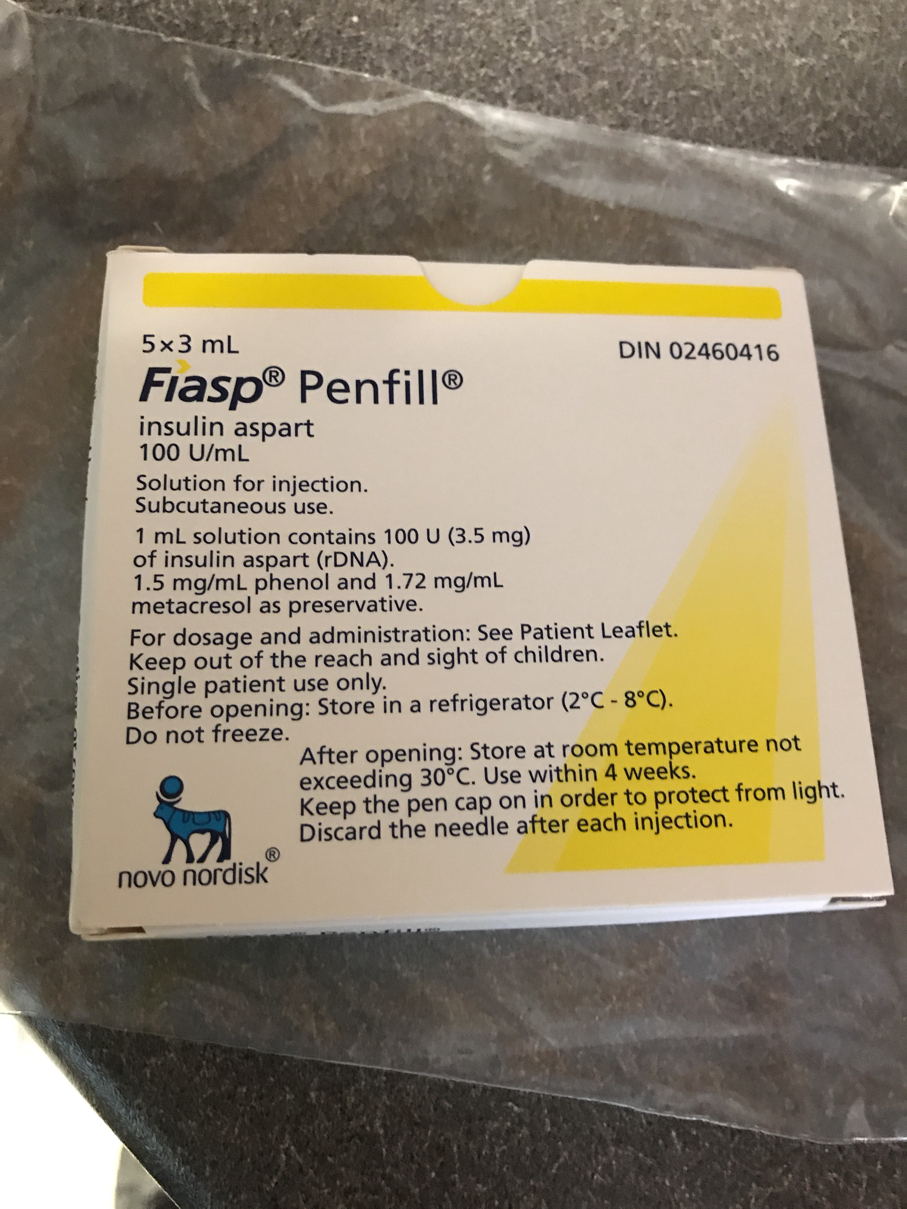
The betes was pretty stable, as I had little appetite and nausea came on/off throughout the hospitalization. This hospital is really good about all things diabetes (I had my son there). This was a huge relief, because that's pretty much my #1 fear, but they have their heads screwed on straight and people are educated and even CDE's visit you (2x) to make sure you know what you're doing should you run the "control insulin" part yourself. I guess mostly to check their little boxes. I had all my d-stuff with me (except for my lancing device,& an extra sensor), the only problem was when my sensor pulled out on the night before discharge(no extra) & when I had to do a pod change the insulin hadn’t come up from the pharmacy yet, so I went a little high.(they gave me an entire vial of Novolog)
Overall, everyone was nice and knowledgeable. One of the techs told me she was glad my blood sugars weren’t like the persons down the hall who was always 400 & then proceeded to go on a rant about how they were uncontrolled and deserved missing limbs. I was in shock with what was coming out of her mouth but really didn’t feel like educating anyone or anything just then. (This is a common opinion in health care settings, just most HCP have the tact not to actually say it to your face. I know this, as a student nurse I got to hear several diatribes on diabetics and couldn’t say anything. I actually now would just rather not hear it.Ticks me off so bad.)
After discharge, I had some pain and swelling of the surgical site (& the surgeons office was not available for follow up for three whole weeks). My primary had to get involved,& there was another CT scan and ER visit and drainage of the area before it finally felt like it was healing. (there was no abcess though, so that much is good) Healing from an appendectomy is no where as simple as they make it out to be-& pain meds will block you up for an entire year,feels like.
But I do feel healed now, & I’m trying to find a job & build a closed loop insulin pump system. (DIY Artificial Pancreas. I’m excited that it will soon be available for Omnipod!)